
Pressure points – The 180/110 report – focus on hypertensive crises in ER
- Hypertension is the leading causes of the global burden of disease
- Affects more than one billion individuals and causes an estimated 9.4 million deaths per year
- Estimated burden of 200 million persons in India
- Age-adjusted hypertension was more in men (24.5%) than women (20.0%)
Definition of hypertension
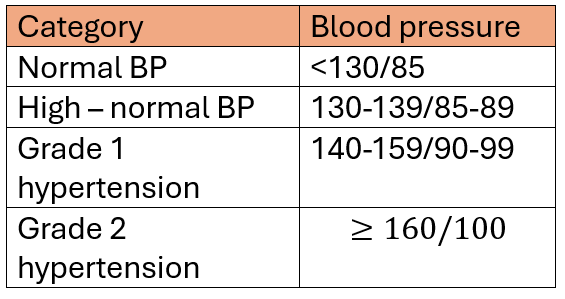
- Systolic blood pressure (SBP) in the office or clinic is ≥140 mm Hg and/or their diastolic blood pressure (DBP) is ≥90 mm Hg following repeated examination
- The diagnosis should not be made on a single office visit
- Usually 2–3 office visits at 1–4-week intervals (depending on the BP level) are required to confirm the diagnosis of hypertension
- The diagnosis might be made on a single visit, if BP is ≥180/110 mm Hg and there is evidence of cardiovascular disease (CVD)
Hypertensive Crisis
- Acute elevation of blood pressure, where the systolic blood pressure is >180 mm Hg and/or the diastolic blood pressure is >120 mm Hg
- Malignant hypertension: Severe BP elevation (commonly >200/120 mm Hg) associated with advanced bilateral retinopathy (hemorrhages, cotton wool spots, papilledema)
- Hypertensive emergency is a hypertensive crisis (systolic blood pressure >180 mm Hg and/or diastolic blood pressure >120 mm Hg) with concomitant end-organ damage
- Hypertensive encephalopathy: Severe BP elevation associated with lethargy, seizures, cortical blindness and coma in the absence of other explanations
- Hypertensive thrombotic microangiopathy: Severe BP elevation associated with hemolysis and thrombocytopenia in the absence of other causes and improvement with BP-lowering therapy
Causes
- Intoxications (e.g., cocaine, amphetamines, phencyclidine hydrochloride, stimulant diet supplements)
- Nonadherence to antihypertensive regimens
- Withdrawal syndromes (e.g., clonidine or β-antagonists)
- Drug -drug/drugfood interactions (e.g., monoamine oxidase inhibitors and tricyclic antidepressants, antihistamines, or tyramine)
- Spinal cord disorders
- Pheochromocytoma
- Pregnancy
- Collagen vascular disease (e.g., systemic lupus erythematosus)
Investigations
- Electrocardiography
- Conventional chest radiography
- Urinalysis
- Serum electrolytes and serum creatinine
- Cardiac biomarkers (if an acute coronary syndrome is suspected)
- Computed tomography (CT) or magnetic resonance imaging (MRI) of the brain (if head injury, neurologic symptoms, hypertensive retinopathy, nausea, or vomiting are present)
- Contrast-enhanced CT or MRI of the chest or transesophageal echocardiography (if aortic dissection is suspected, although rapid blood pressure lowering need not be delayed in such patients while awaiting the results of imaging)
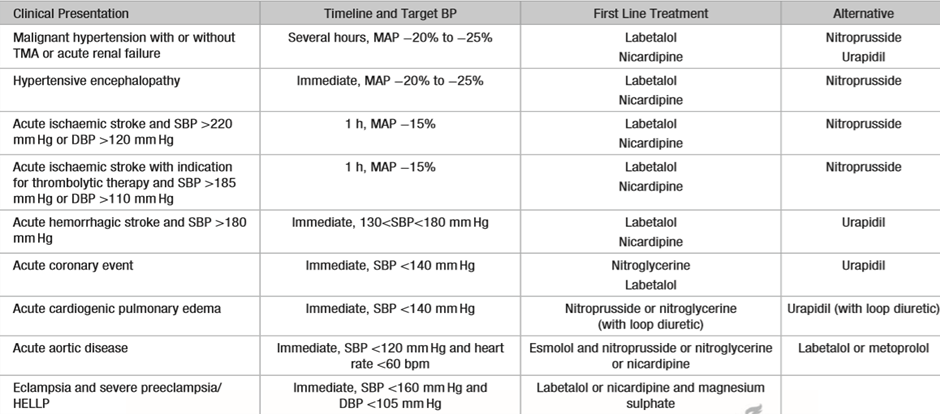
Treatment goals
- The treatment target for hypertensive urgency is a gradual blood pressure reduction over 24–48 hours
- For most hypertensive emergencies, mean arterial pressure should be reduced gradually by approximately 10 to 20 percent in the first hour and by a further 5 to 15 percent over the next 23 hours
- This often results in a target blood pressure of <180/<120 mmHg for the first hour and <160/<110 mmHg for the next 23 hours
References
◦ Rajeev Gupta, Venkata Ram. Hypertension Epidemiology in India: Emerging aspects. Curr opin cardiol. 2019Jul;34(4):331-341.
◦ Jayanthi Chandar, Gastón Zilleruelo. Hypertensive crisis in children. Pediatr Nephrol. (2012) 27:741–75.
◦ 2020 International Society of Hypertension Global Hypertension Practice Guidelines
◦ Tintinallis emergency medicine, a comprehensive study guide, 9th edition
◦ Harrison’s principles of internal medicine 20th edition

Leave a Reply